Ulcerative colitis (UC) is a persistent ailment impacting the large intestine and rectum, marked by inflammation and ulceration of the inner lining of these organs. Common symptoms of UC encompass diarrhea, blood in the stool, abdominal pain and cramping, as well as weight loss. The precise cause of UC remains unidentified, though it is thought to be a result of a combination of genetic, environmental, and immune factors.
What is UC medical term?
UC, short for Ulcerative Colitis, represents a form of inflammatory bowel disease characterized by inflammation and ulcers in the lining of the large intestine and rectum. In the medical field, UC is employed as an abbreviation for Ulcerative Colitis when discussing the condition in a clinical context.
Diagnosis of UC involves a combination of a physical examination, blood tests, stool tests, and imaging studies such as colonoscopy or CT scan. Treatment typically includes medications like aminosalicylates, corticosteroids, immunomodulators, and biologic agents, alongside lifestyle adjustments such as a high-fiber diet and stress management. In some instances, surgery may be required to remove the affected part of the colon.
It’s important to distinguish UC from Crohn’s disease, another form of inflammatory bowel disease (IBD) that can impact any segment of the digestive tract, not solely the colon.
How is UC diagnosed?
Coping with UC presents challenges as its symptoms can be incapacitating, significantly affecting an individual’s quality of life. Those with UC may contend with fatigue, anemia, and malnutrition resulting from chronic diarrhea and blood loss. Moreover, the persistent nature of the disease may contribute to emotional and psychological distress, manifesting as conditions like depression and anxiety.
Collaborating closely with a healthcare team is crucial for individuals with UC to effectively manage symptoms and avert complications. This involves routine check-ups, monitoring medication side effects, and adjusting treatments as necessary.
Diet and nutrition play pivotal roles in UC management. A high-fiber diet can aid in preventing constipation and diarrhea. Some individuals may need to eliminate specific trigger foods, such as spicy or high-fat items, to alleviate symptoms. Maintaining adequate hydration is essential to counteract potential dehydration, particularly for those dealing with chronic diarrhea.
Physical activity holds significance for individuals with UC. Regular exercise contributes to overall health improvement, stress reduction, and anxiety alleviation. Before initiating a new exercise regimen, especially during symptom flare-ups, it’s essential to consult with a healthcare provider.
In summary, living with UC entails navigating a prolonged and intricate journey. However, with effective management and a supportive environment, individuals with UC can lead fulfilling lives.
What causes UC disease?
The precise cause of Ulcerative Colitis (UC) remains elusive, with current understanding pointing to a blend of genetic and environmental factors. Researchers theorize that an erroneous response from the immune system leads to an attack on colon cells, resulting in inflammation and ulcers. Additional potential contributors may encompass alterations in the gut microbiome, viral or bacterial infections, and exposure to specific environmental toxins.
Ulcerative Colitis:
Causes and Risk Factors Ulcerative colitis occurs when the immune system malfunctions, mistaking harmless elements in the body, such as food, beneficial gut bacteria, and colon lining cells, as threats. This leads to an attack by white blood cells on the colon lining, resulting in inflammation and ulcers.
The exact cause of ulcerative colitis is unknown, but genetic factors likely play a role, as the condition can run in families. Other environmental factors may also contribute.
Factors that may affect your risk of developing ulcerative colitis include:
- Age: The condition is more common in individuals aged 15 to 30 and those over 60.
- Ethnicity: People of Ashkenazi Jewish descent are at a higher risk.
- Family History: Having a close relative with ulcerative colitis can increase your risk by up to 30%.
While food and stress do not directly cause ulcerative colitis, they can trigger symptom flare-ups.
Types of Ulcerative Colitis
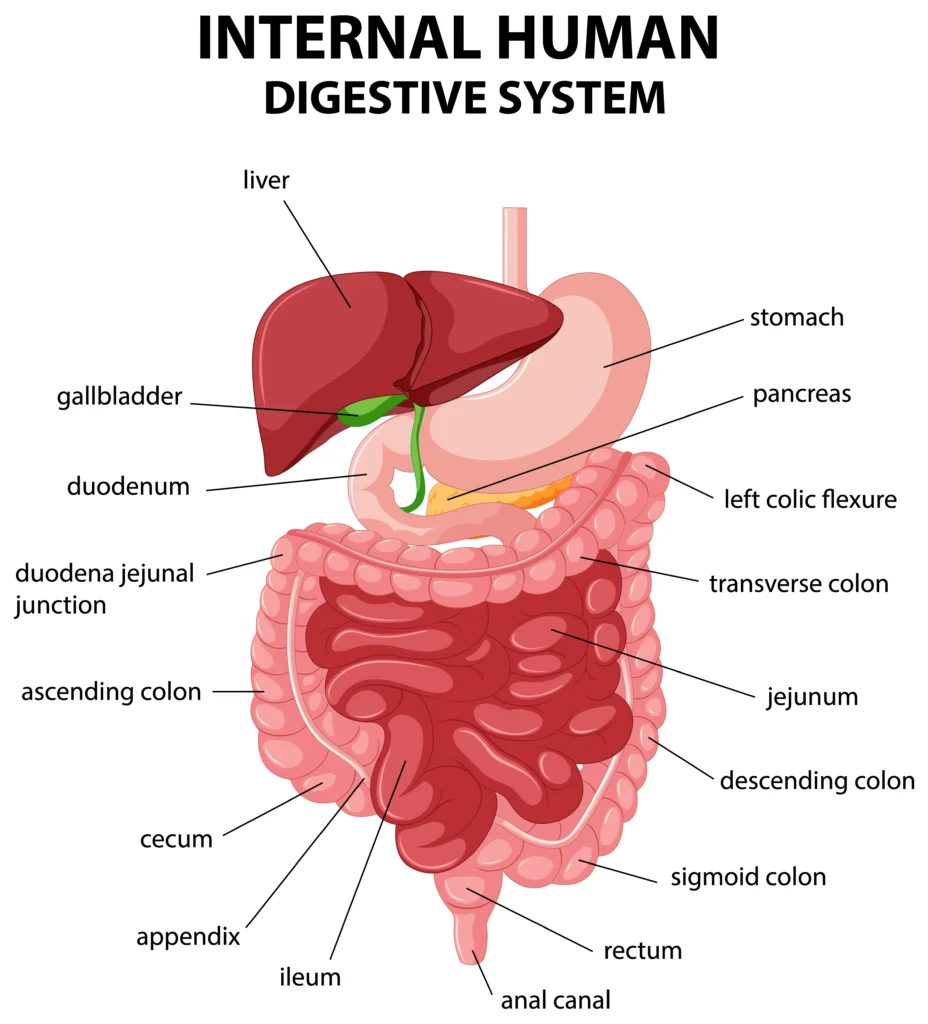
Ulcerative colitis can vary in severity and location within the colon. The specific type you have depends on where the inflammation occurs:
Ulcerative Proctitis: This is the mildest form and affects only the rectum, causing symptoms such as rectal bleeding.
Proctosigmoiditis: Involves inflammation in the rectum and the sigmoid colon (lower end of the colon), leading to symptoms like bloody diarrhea, abdominal cramps, and tenesmus (the urge to pass stool with little or no stool actually passing).
Left-sided Colitis: Inflammation extends from the rectum up through the left side of the colon, causing cramps on the left side of the abdomen, bloody diarrhea, and unintended weight loss.
Pancolitis: Affects the entire colon and can result in severe bouts of bloody diarrhea, abdominal cramps, pain, fatigue, and significant weight loss.
Acute Severe Ulcerative Colitis: This is a rare form that affects the entire colon and causes severe symptoms such as intense pain, heavy diarrhea, rectal bleeding, and fever.
Ulcerative Colitis Symptoms
| Symptom | Description |
|---|---|
| Bloody diarrhea | Main symptom of ulcerative colitis, often with pus in stools |
| Cramping abdominal pain | Common abdominal discomfort |
| Sudden urges to have a bowel movement | Urgent need to pass stools suddenly |
| Loss of appetite | Decreased desire to eat |
| Unintended weight loss | Weight loss without trying |
| Fatigue | Feeling of extreme tiredness |
| Fever | Elevated body temperature |
| Dehydration | Excessive loss of body fluids |
| Joint pain or soreness | Pain or discomfort in the joints |
| Canker sores | Small, painful ulcers in the mouth |
| Eye pain when exposed to bright light | Sensitivity to light accompanied by eye pain |
| Anemia (too few red blood cells) | Reduced red blood cell count |
| Skin sores | Sores or lesions on the skin |
| Sensation of incomplete bowel emptying | Feeling that the bowel has not emptied completely after a bowel movement |
| Nighttime bowel movements | Need to pass stools during the night |
| Incontinence | Inability to control bowel movements, leading to involuntary leakage |
| Pain or bleeding during bowel movements | Discomfort or blood in stools during bowel movements |
| Fluctuating symptoms | Symptoms may flare up, improve, and reappear intermittently, with periods of remission and flare-ups over time. |
Comparison of Ulcerative Colitis, Crohn's Disease, and Irritable Bowel Syndrome
| Characteristic | Ulcerative Colitis | Crohn’s Disease | Irritable Bowel Syndrome |
|---|---|---|---|
| Area of Effect | Large intestine (colon) and its lining | Any part of the digestive tract | Muscles in the intestines |
| Inflammation | Limited to the large intestine | Can occur anywhere in the digestive tract | No inflammation or ulcers |
| Ulcers | Present | Can be present, but not always | No ulcers |
| Symptoms | Bloody diarrhea, abdominal pain | Similar symptoms, but may include | Similar symptoms, but not due to |
| other complications like strictures, | inflammation or ulcers | ||
| fistulas, or abscesses | |||
| Diagnosis | Colonoscopy and biopsy | Imaging tests, colonoscopy, and | Based on symptoms and ruling out |
| biopsy | other conditions | ||
| Treatment | Medications, diet changes, surgery | Medications, diet changes, surgery | Symptom management, diet changes, |
| stress management | |||
| Commonality | Less common | Less common | Common |
Ulcerative Colitis Diagnosis: Tests and Procedures to Confirm UC
To diagnose ulcerative colitis (UC) and distinguish it from other gut diseases, your doctor may conduct several tests and procedures:
Blood tests: These can reveal signs of anemia or inflammation in your body.
Stool samples: Your doctor may analyze stool samples to rule out infections or parasites in your colon. This test can also detect hidden blood in your stool.
- Flexible sigmoidoscopy: During this procedure, a flexible tube with a camera and light is inserted into your lower colon through your rectum. Your doctor may also take a small tissue sample (biopsy) for further examination.
- Colonoscopy: Similar to flexible sigmoidoscopy but examines your entire colon. This procedure allows your doctor to visualize the extent and severity of inflammation.
- X-rays: While less common, X-rays may be used in certain situations to diagnose UC.
These tests and procedures help your doctor accurately diagnose ulcerative colitis and develop an appropriate treatment plan.
Ulcerative Colitis Treatment Options
Treatment for ulcerative colitis (UC) aims to alleviate symptoms, promote colon healing, and prevent future flare-ups. Your treatment plan may include a combination of dietary adjustments, medications, and in some cases, surgery.
Diet: Certain foods can exacerbate symptoms. A diet consisting of soft, bland foods may be easier on your digestive system than spicy or high-fiber foods. If you are lactose intolerant, your doctor may recommend avoiding dairy products. A balanced diet rich in fiber, lean protein, fruits, and vegetables can provide essential nutrients.
Medications: Your doctor may prescribe various medications, including:
- Antibiotics: These help fight infections and promote healing in the large intestine.
- Aminosalicylates: These contain 5-aminosalicylic acid (5-ASA), which reduces inflammation and manages symptoms. They may be administered orally or as enemas/suppositories.
- Corticosteroids: If aminosalicylates are ineffective or if symptoms are severe, corticosteroids may be prescribed for a short duration to reduce inflammation.
- Immunomodulators: These medications help suppress the immune system’s attack on the colon. They may take several months to show significant effects.
- Biologics: Derived from living cell proteins, biologics are reserved for severe cases of UC.
- Janus kinase inhibitors (JAK inhibitors): Oral medications that can induce and maintain remission in ulcerative colitis.
- Sphingosine 1-phosphate (S1P) receptor modulators: Oral medication for patients with moderate to severe UC.
- Loperamide: Helps control diarrhea, but should be used under the guidance of a doctor.
Surgery: If conservative treatments fail or if UC is severe, surgery may be necessary. Procedures such as colectomy (removal of the colon) or proctocolectomy (removal of the colon and rectum) may be performed. In a proctocolectomy, a small pouch made from the small intestine may be created and connected to the anus (ileal pouch-anal anastomosis) to enable normal waste expulsion without the need for a collection bag.
Your doctor will tailor a treatment plan based on the severity of your condition and your individual needs to effectively manage ulcerative colitis.
Complications of Ulcerative Colitis
Ulcerative colitis can lead to several complications, including:
Bleeding: Chronic inflammation in the colon can cause bleeding, leading to anemia.
Osteoporosis: Weakness in bones may occur due to dietary deficiencies or prolonged corticosteroid use.
Dehydration: Severe inflammation in the colon can hinder the absorption of fluids, necessitating intravenous fluid administration.
Extra-intestinal Inflammation: Inflammation associated with UC can affect other parts of the body, including the joints, skin, and eyes.
Fulminant Colitis: In severe cases, UC can cause the colon to rupture or lead to systemic infection, causing abdominal swelling and cessation of bowel movements.
Megacolon: Fulminant colitis can result in severe swelling or rupture of the large intestine, often requiring surgical intervention.
Liver Complications: Inflammation of the bile ducts or liver, as well as the development of liver scar tissue, can occur.
Colon Cancer: Individuals with ulcerative colitis are at an increased risk of developing colon cancer, particularly if the entire colon is affected or if UC has been present for an extended period.
Questions to Ask Your Doctor About Ulcerative Colitis
Whether you suspect you have ulcerative colitis (UC) or have already been diagnosed and seek further information, consider asking your doctor the following questions:
- Is my condition indicative of ulcerative colitis (UC), or could it be another ailment?
- Are there different types of UC, and do they present with varying symptoms?
- Which diagnostic tests are necessary for confirmation?
- What treatment plan do you recommend if I am diagnosed with ulcerative colitis?
- Can modifications to my diet or lifestyle help alleviate my symptoms?
- How severe is my ulcerative colitis?
- What are the potential side effects of the prescribed medication for my ulcerative colitis?
- Should I consider taking nutritional supplements, such as probiotics?
- How frequently should I schedule follow-up appointments?
- What steps should I take if my symptoms suddenly worsen?
- What are the signs indicating a worsening condition of my ulcerative colitis?
- When should I consider changing my ulcerative colitis medication?
- Is surgery a viable option for me, and what does the procedure entail?
- What is my risk of developing colon cancer due to ulcerative colitis?
Ulcerative Colitis Outlook
Ulcerative colitis typically manifests as a chronic, or long-lasting, condition for most individuals. It is characterized by episodes of flares and periods of remission, during which no symptoms are present. While a small percentage of individuals experience a single episode and remain symptom-free thereafter, approximately 10% of those with UC encounter a rapid deterioration after the initial attack, leading to severe complications.
Over time, the disease progresses to involve the entire large intestine in many cases. This escalation can elevate the risk of developing colon cancer. However, if the disease is detected early and the colon is surgically removed, about half of the affected individuals survive.
FAQ's
What is ulcerative colitis?
Ulcerative colitis is a chronic inflammatory bowel disease that causes inflammation and ulcers in the inner lining of the colon and rectum.
What are the symptoms of ulcerative colitis?
Symptoms of ulcerative colitis can include abdominal pain, bloody diarrhea, fatigue, weight loss, and dehydration.
What causes ulcerative colitis?
The exact cause of ulcerative colitis is unknown, but it is believed to involve a combination of genetic, environmental, and immune system factors.
How is ulcerative colitis diagnosed?
Diagnosis of ulcerative colitis typically involves a combination of medical history, physical examination, blood tests, stool tests, colonoscopy, and imaging tests.
What are the treatment options for ulcerative colitis?
Treatment for ulcerative colitis may include medications such as anti-inflammatory drugs, immune system suppressors, and biologics, as well as dietary and lifestyle changes. In severe cases, surgery to remove the colon may be necessary.
Can ulcerative colitis be cured?
There is currently no cure for ulcerative colitis, but treatment can help manage symptoms and improve quality of life.
What complications can arise from ulcerative colitis?
Complications of ulcerative colitis can include severe bleeding, perforation of the colon, increased risk of colon cancer, and osteoporosis.
How can I manage ulcerative colitis?
Managing ulcerative colitis involves working closely with your healthcare team, taking prescribed medications, following a healthy diet, managing stress, and avoiding trigger foods.
Can ulcerative colitis affect pregnancy?
Yes, ulcerative colitis can affect pregnancy. It is important for women with ulcerative colitis to work closely with their healthcare providers to manage their condition during pregnancy.
What should I do if I suspect I have ulcerative colitis?
If you suspect you have ulcerative colitis, it is important to see a healthcare provider for a proper diagnosis and treatment plan. Do not self-diagnose or self-treat.



